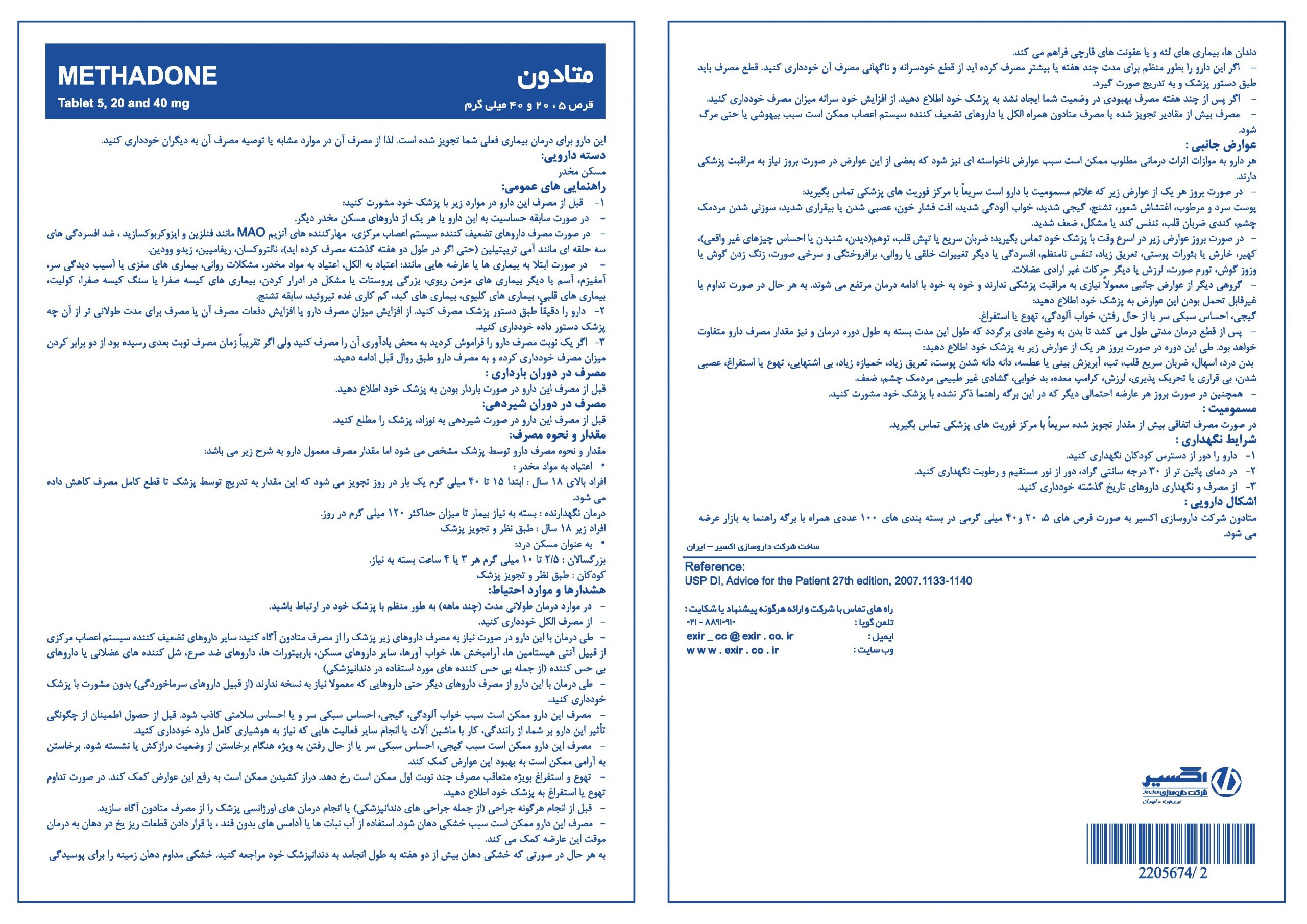
METHADONE 5 mg
tablet Methadone 5 mg

| Generic Name of Product | Brand Name | Dosage Form | Strength | Pharmacologic Group | Therapeutic Group | Unit Per Pack |
| Methadone | - | Tablet | 5mg, 20mg, 40mg | Narcotic analgesics | Narcotics | 100 |
Indications And Usage | Management of pain severe enough to require daily, around-the-clock, long-term opioid treatment and for which alternative treatment options are inadequate. Detoxification treatment of opioid addiction (heroin or other morphine-like drugs). Maintenance treatment of opioid addiction (heroin or other morphine-like drugs), in conjunction with appropriate social and medical services. | ||||||||||||||||
Administration | Methadone Hydrochloride Oral Solution should be prescribed only by healthcare professionals who are knowledgeable in the use of potent opioids for the management of chronic pain. Consider the following important factors that differentiate methadone from other opioid analgesics: There is high interpatient variability in absorption, metabolism, and relative analgesic potency of methadone. The duration of analgesic action of methadone is 4 to 8 hours (based on single-dose studies) but the plasma elimination half-life is 8 to 59 hours. With repeated dosing, the potency of methadone increases due to systemic accumulation. Steady-state plasma concentrations, and full analgesic effects, are not attained until at least 3 to 5 days on a dose, and may take longer in some patients. Use of Methadone Hydrochloride Tablets as the First Opioid Analgesic: Initiate treatment with Methadone Hydrochloride Tablets with 2.5 mg orally every 8 to 12 hours. Conversion from Other Oral Opioids to Methadone Hydrochloride Tablets: Discontinue all other around-the-clock opioid drugs when Methadone Hydrochloride Tablets therapy is initiated. Deaths have occurred in opioid-tolerant patients during conversion to methadone. Conversion Factors to Methadone Hydrochloride Tablets:
| ||||||||||||||||
Contraindications | Significant respiratory depression Acute or severe bronchial asthma in an unmonitored setting or in the absence of resuscitative equipment Known or suspected gastrointestinal obstruction, including paralytic ileus Hypersensitivity (e.g., anaphylaxis) to methadone | ||||||||||||||||
Precautions | Risk of Accidental Overdose and Death due to Medication Errors, Addiction, Abuse and Misuse, Opioid Analgesic Risk Evaluation and Mitigation Strategy (REMS), Life-Threatening Respiratory Depression, Life-Threatening QT Prolongation6 Neonatal Opioid Withdrawal Syndrome, Risks of Concomitant Use of Cytochrome P450 3A4, 2B6, 2C19, 2C9, or 2D6 Inhibitors or Discontinuation of P450 3A4, 2B6, 2C19, or 2C9 Inducers, Risks from Concomitant Use with Benzodiazepines or Other CNS Depressants, Life-Threatening Respiratory Depression in Patients with Chronic Pulmonary Disease or in Elderly, Cachectic, and Debilitated Patients, Serotonin Syndrome with Concomitant Use of Serotonergic Drugs, Adrenal Insufficiency, Severe Hypotension, Risks of Use in Patients with Increased Intracranial Pressure, Brain Tumors, Head Injury, or Impaired Consciousness, Risks of Use in Patients with Gastrointestinal Conditions, Increased Risk of Seizures in Patients with Seizure Disorders, Withdrawal, Risks Driving and Operating Machinery, Laboratory Test Interactions | ||||||||||||||||
Adverse Reactions | Addiction, Abuse, and Misuse, Life Threatening Respiratory Depression, QT Prolongation, Neonatal Opioid Withdrawal Syndrome, Interactions with Benzodiazepines and other CNS Depressants, Serotonin Syndrome, Adrenal Insufficiency, Severe Hypotension, Gastrointestinal Adverse Reactions, Seizures, Withdrawal | ||||||||||||||||
Pregnancy and lactation | Neonatal opioid withdrawal syndrome (NOWS) is an expected and treatable outcome of prolonged use of opioids during pregnancy. There are no adequate and well-controlled studies in pregnant women. | ||||||||||||||||
Renal and liver Impairment | Methadone pharmacokinetics have not been extensively evaluated in patients with hepatic insufficiency. Methadone is metabolized by hepatic pathways; therefore, patients with liver impairment may be at risk of increased systemic exposure to methadone after multiple dosing. Start these patients on lower doses and titrate slowly while carefully monitoring for signs of respiratory and central nervous system depression.
Methadone pharmacokinetics have not been extensively evaluated in patients with renal insufficiency. Since un metabolized methadone and its metabolites are excreted in urine to a variable degree, start these patients on lower doses and with longer dosing intervals and titrate slowly while carefully monitoring for signs of respiratory and central nervous system depression. | ||||||||||||||||
Laboratory Tests | Monitor patients closely for respiratory depression, especially within the first 24 to 72 hours of initiating therapy and following dosage increases with Methadone Hydrochloride. |